
Updated 2023/09/14.
The implications of cumulative SARS-CoV-2 infections are forming an ever-worsening picture, while the California Supreme Court just ruled that an employer could not be held liable for the infection of an employee who went on to infect his wife. The court explained that this is because it would set a precedent that would bring the economy to its knees, stating that "finding a duty to care" would have been the moral thing to do, but ultimately admitting that the economy is not — and cannot — be moral. The court wrote:
In sum, while the foreseeability factors and the policy factor of moral blame largely tilt in favor of finding a duty of care, the policy factors of preventing future harm and the anticipated burdens on defendants and the community weigh against imposing such a duty. Some factors may be so weighty as to tip the balance one way or the other. Here, the significant and unpredictable burden that recognizing a duty of care would impose on California businesses, the court system, and the community at large counsels in favor of an exception to the general rule of Civil Code section 1714 [emphasis added].
Imposing on employers a tort duty to each employee’s household members to prevent the spread of this highly transmissible virus would throw open the courthouse doors to a deluge of lawsuits that would be both hard to prove and difficult to cull early in the proceedings. Although it is foreseeable that employees infected at work will carry the virus home and infect their loved ones, the dramatic expansion of liability plaintiffs' suit envisions has the potential to destroy businesses and curtail, if not outright end, the provision of essential public services.
The basis for declaring the public health emergency over was the decline in acute deaths and hospitalizations, while the Omicron lineage has evolved to be even more neuroinvasive, producing a host of extremely concerning neurological outcomes. This is all being documented in peer-reviewed journals that medical doctors are apparently not keeping up with, because masks are a thing of the past in hospitals, Australia has recorded more than 600 deaths due to hospital-acquired covid, and Harvard's Bill of Health blog is wondering when this will be considered malpractice.
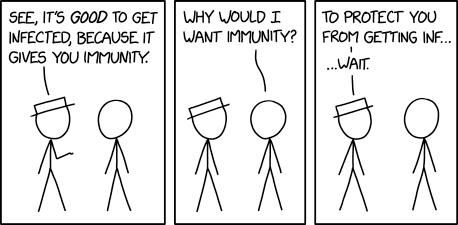
The myth that the immune system is like a muscle that needs to be used to stay in shape is as popular as ever, while the complete opposite is true: there is no material benefit to any amount of viral infections, and the immune system stays healthier for longer the less it is engaged. Playing in the dirt as kids was for exposure to commensal bacteria, not viruses. SARS-CoV-2 in particular causes lasting immune dysfunction in 10-30% of intfected people — odds that do not improve with reinfection. It may even be the case that this is a universal feature of SARS-CoV-2.
 All while — in the United States — covid is the eighth leading cause of death in children and adolescents, the number one driver of pediatric diabetes, the third leading cause of death for all ages, and directly contributes to the number one cause of death (heart disease).
All while — in the United States — covid is the eighth leading cause of death in children and adolescents, the number one driver of pediatric diabetes, the third leading cause of death for all ages, and directly contributes to the number one cause of death (heart disease).
I have been told, "perhaps," and that I would be thought of during this "troubling time," in response to the statement that turning public health into personal choice upholds the logic of eugenics. The level of understatement is dizzying.
I told the CEO of a behavioral health nonprofit that the least that could be done to mitigate the spread of covid through their therapy rooms was the installation of HEPA air purifiers in each room, and was told that upkeep would be too expensive. The inability to rationalize prevention as cheaper than treatment — or lost labor as employees become sick — is even more dizzying.
With invisible threats like airborne disease, warnings necessarily focus on preventing certain outcomes, which means preventing visible indicators of those outcomes. Folks don't realize when they are succeeding at preventing outcomes that they never end up seeing, so there ends up being a self-reinforcing "I need to see it to believe it" problem until the consequences pile up to an undeniable degree.
You can see wildfire smoke — its immediate effects on the eyes and throat and lungs are obvious, and it's not hard to convince people to put on a respirator when the smoke is so thick that the sun is red. Even if they wouldn't think to do so themselves, it's an easier sell. But with an airborne disease that can take time to fully manifest its complications, people let doubt win, especially if they can confuse those long-term complications for something else, or blame something that feels more concrete to them.
Maybe we need better analogies. Imagine if 1 out of every 10 times you get in your car, you end up in a car crash. Maybe you emerge with minor injuries, maybe you end up disabled for life. As you begin the process of healing, you keep getting in your car, and before you've had a chance to fully heal from the previous one, you end up in another car crash.
Any way you portray it, normalcy bias gets in the way of the precautionary principle's attempt to avoid worst-case scenarios, until there is an ultimately-preventable — but undeniable and paradigm-shifting — mountain of disability and death. When the stakes are human and the precautions feel inhuman, this tendency is powerful. In 1975, the Panel on the Public Policy Implications of Earthquake Prediction defined it as "the tendency for people to accept most readily any information that enables them to disbelieve the prediction, minimize the danger, and view the situation optimistically."

The basic expectation that infection is inevitable can be found in headlines like National Geographic's that ask, "The EG.5 COVID variant is spiking in the U.S. Is it time to mask up?" But if you are someone interested in interrupting chains of transmission, it is never not time to mask up. If you are truly embracing the idea of endemicity, it will always be time to mask up, because that's appropriate endemic behavior. Imagine asking "is it time for mosquito nets?" while malaria is spiking.
Simply put, only putting on a mask when cases are rising is precisely how they rise in the first place. Masking when cases are lower is how they stay lower.
The most egregious thing about doctors no longer wearing masks as a universal precaution is that they are many peoples' most immediate role model in terms of anything public health-related. If their doctor doesn't care, why should they? Meanwhile, authors of an article published in Infection Control & Hospital Epidemiology back in February have argued for "permanently including universal masking in routine patient-care interactions."
What we are facing is an iteration of the Semmelweis reflex-effect, named after the reaction to Ignaz Philipp Semmelweis, an Austrian physician who — in the 1840s — had a hunch that what he called "cadaverous particles" were being transferred from cadavers to newborns by the hands of doctors who had touched those cadavers. From the National Infectious Disease Prevention Initiative at Ohio State University:
Semmelweis decided to act on his hunch. He instituted a clinic-wide policy of mandatory hand washing between cutting up a body and assisting in a birth. [...] In the first three months, death rates plummeted from one in ten to one in a hundred. Semmelweis had shown that he could conquer childbed fever with handwashing.
Or so you’d think. In fact, Semmelweis’ arguments were completely rejected by the medical establishment at the time. Coming decades before Pasteur’s germ theory of disease, and without a strong theoretical explanation, his actions seemed to be a reversion to the "speculative theories of earlier decades that were so repugnant to his positivist contemporaries."
[...] To be fair, Semmelweis did have major faults in his reasoning — he thought that only cadaverous particles caused the fever, and couldn’t explain why some women still contracted fever in the midwife clinic. But, perhaps most importantly, his theories presented a behavioral conundrum for his fellow physicians: testing his hypothesis further could implicate them as dealers of death. Accusing doctors of haplessly causing disease was a slur on the gentlemanly art of medical practice.
Such resistance within the medical community was short-lived. In the later part of the 19th century, a rising tide of empiricism — in particular the work of Joseph Lister and Louis Pasteur — lifted the lonely little ship of hygiene, and the benefits of hand washing would become universally accepted.
It happened with cholera, too. From The John Snow Project:
In 1854, Dr John Snow figured out what nobody else had: the people dying from Cholera were all drinking the same water. He managed to convince the authorities to remove the handle from the Broad Street water pump. Sure enough, people stopped dying. It turns out the water was polluted by sewage. His discovery eventually led to clean water in cities all over the world, changing public health forever.
Except soon after the immediate threat had subsided, the authorities decided to replace the pump handle. They had no idea if the water was safe. They ignored the one thing that stopped the spread — not drinking water full of shit. Lessons learned were quickly ignored, and in 1866 the disease spread in the water again, killing thousands.
Perhaps the best analogy of all is from artist Amandu Hu:
Given the timeline from the rise of its ubiquity (early 1800s), scientists connecting smoking to lung cancer (1900), tobacco companies acknowledging it internally (1952), but only 1/3 of doctors thought it was definitive (1960), to mass acknowledgement (1990s) and bans inside (2003 in Canada), I’d say we’ve gone from 1800 to 1960 in 3 years. The evidence is mounting that covid is harmful long-term. The standards for buildings and shared spaces are changing. Behaviour follows.
We are in the tricky time period when you might have known smoking is harmful, but we still had unpartitioned smoking/non-smoking sections. If you didn’t want to breathe in smoke, people thought you were weird or a buzzkill because you refused eat in restaurants.
We are not going back to pre-pandemic life. Now is the time to really focus on surviving while the rest of the world catches up. Note: workers who could not choose to avoid bad conditions or social pressures bore the greatest cost of smoking. That’s why covid safety should be a key worker issue.
Sooner or later people will need to accept that the world has been permanently changed by the presence of an airborne chronic illness generator, which is traumatic and requires grief processing. The people starting this grieving process early are being pariahed by a worldview impasse at the heart of a deeply-embedded ableism and entitlement rift, which is passively enabling survivorship bias at sunk-cost scale. How long will it take the world to catch up this time?
***
"Obligations
Complications
Routines and schedules
The drug that will kill you
Kill you
Oh, you"
- Radiohead
References:
- [Open-Source Eschaton] – Covid Fact Sheet
-
The Supreme Court of California – Corby Kuciemba v. Victory Woodworks, Inc (PDF)
- California Law – Civil Code, Division 3, Part 3, Section 1714
- [Open-Source Eschaton] – Why Ending the Public Health Emergency Declaration is a Bad Idea
- FRED – Population - With a Disability, 16 Years and over
- The Age – Hundreds die of COVID after catching virus while in hospital
- Bill of Health – Hospitals That Ditch Masks Risk Exposure
- The John Snow Project – COVID-19: A New Disease Paradigm
- Bill of Health – The Current COVID-19 Surge, Eugenics, and Health-Based Discrimination
- Journal of the Saudi Heart Association – Physician ‘defiance’ towards hand hygiene compliance: Is there a theory–practice–ethics gap?
- ScienceDirect – Precautionary Principle
- Thomas E. Drabek via Sci-Hub [PDF] – Human System Responses to Disaster: An Inventory of Sociological Findings
- National Geographic – The EG.5 COVID variant is spiking in the U.S. Is it time to mask up?
- Infection Control & Hospital Epidemiology – Back to the future: Redefining “universal precautions” to include masking for all patient encounters
- National Infectious Disease Prevention Initiative – The Dirty History of Doctors’ Hands
- The John Snow Project – About
-
@amandahu via Twitter (via Threadreader) – "... changing attitudes about smoking in our society and parallels to COVID"
- Tobacco Control – The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll
- Midnight Sun – Why Has the Left Deprioritized COVID?
- Epidemiology and Psychiatric Sciences – Uncovering survivorship bias in longitudinal mental health surveys during the COVID-19 pandemic
