Updated 2025/01/12.
Note: this is not an anti-vaccine piece. The mRNA and protein-based covid vaccines are extremely important as a base-layer precaution. However, they are not – in their current form, and on their own – enough to end the pandemic. They mitigate, but do not fully prevent the ongoing harms of SARS-CoV-2. Non-pharmaceutical interventions – like respirator use, air filtration/ventilation, and air sterilization/disinfection – remain necessary.
Outline:
- The vaccines do not prevent infection.
- The vaccines do not prevent transmission.
- The vaccines do not induce antibodies in a significant amount of vulnerable people, and do not appear to induce long-lived antibodies in anyone.
- The rate of SARS-CoV-2 mutation is exponential, and breakthrough infections do not always induce antibodies/hybrid immunity.
- Infection impairs the CD8+ T cell response to vaccination, and breakthrough infections dysregulate T cells.
- Breakthrough infections are not harmless.
- People who cannot access, fully benefit from, or tolerate the vaccines matter.
1. The vaccines do not prevent infection.
On August 27, 2021, the CDC reported in their Morbidity and Mortality Weekly Report series that "during December 14, 2020 [to] April 10, 2021, data [...] among frontline workers [...] showed that the Pfizer-BioNTech and Moderna mRNA COVID-19 vaccines were approximately 90% effective in preventing symptomatic and asymptomatic infection with SARS-CoV-2, the virus that causes COVID-19, in real-world conditions."
This was determined by "test[ing] weekly for SARS-CoV-2 infection by reverse transcription-polymerase chain reaction (RT-PCR) and upon the onset of any COVID-19-like illness." This data was reportedly "adjusted for occupation, site, and local viral circulation, and weighted for inverse probability of vaccination using sociodemographic characteristics, health information, frequency of close social contact, and mask use."
Despite 1 in 10 breakthroughs – a significant amount – that's pretty impressive. However, this is the only of the CDC's reports that mentions vaccines preventing asymptomatic infection. Each report since is careful to specify symptomatic infection.
Similarly, the CDC's Vaccine Effectiveness Studies page specifies that preventing symptomatic infection is an outcome of interest for covid vaccine policy – not asymptomatic infection.
2. The vaccines do not prevent transmission.
Once the confidence that vaccines could prevent infection disappeared, the burden of proof that they could prevent transmission was never met.
In August 2021, the CDC published a report from the Massachusetts Department of Public Health, which found outbreaks among fully vaccinated residents attending large public gatherings in Barnstable County, Massachusetts the month before.
In February 2022, the journal Lancet Infectious Diseases published a study by researchers at the Imperial College London, which found that "fully vaccinated individuals with breakthrough infections have peak viral load similar to unvaccinated cases and can efficiently transmit infection in household settings, including to fully vaccinated contacts," despite the virus clearing faster from the upper airways.
In January 2023, the journal Nature Medicine published a study by researchers at UCSF and UCB, which found that – between December 2021 and May 2022, across 35 California state prisons – "SARS-CoV-2 breakthrough infections and reinfections remained highly infectious and were responsible for 80% of transmission observed in the study population, which has high levels of both prior infection and vaccination. This observation underscores that vaccination and prevalent naturally acquired immunity alone will not eliminate risk of SARS-CoV-2 infection, especially in higher-risk settings, such as prisons."
3. The vaccines do not induce antibodies in a significant amount of vulnerable people, and do not appear to induce long-lived antibodies in anyone.
In August 2022, the journal Annals of Allergy, Asthma & Immunology published a study by researchers at Mayo Clinic, which found that "22.7% of patients failed to seroconvert, with most of these patients either having cancer or B cell depletion therapies."
In the same month, Virology Journal published a review article by researchers at the Tehran University of Medical Sciences and the University of Pittsburgh, which found that 42.89% of a pooled sample of 13,181 immunocompromised patients did not produce antibodies after a second dose of an mRNA vaccine. Out of 909 organ transplants who received a third dose, 51.35% did not produce antibodies. The review also clarifies the rising odds of seroconversion after the second dose (57.11% vs 26.17%), and that the only study population receiving a third dose were organ transplant patients. This underscores the necessity of successive doses to increase the overall odds of vaccine seroconversion in immunocompromised populations.
In September 2024, the journal Nature Medicine published a study by researchers at Emory University, which found that "SARS-CoV-2-specific plasma cells" – or antibody-producing cells – "are not durably established in the bone marrow long-lived compartment after mRNA vaccination," and that "the inherent nature of the spike protein itself may be an issue in B cell activation since neutralizing antibody responses to seasonal human coronaviruses, as well as to SARS-CoV-1 and MERS-CoV, are also short-lived."
4. The rate of SARS-CoV-2 mutation is exponential, and breakthrough infections do not always induce antibodies/hybrid immunity.
In April 2023, the journal Vaccine published a study by researchers from multiple universities, institutes, and clinics in Maryland and North Carolina, which found that – after adjusting for covariates – an estimated 11.2% of people between March and October of 2021 did not produce antibodies following breakthrough infections.
In July 2022, the journal Nature Microbiology published a study by researchers from multiple universities and clinics in the UK, which found, "using sera from double-vaccine recipients, [that] Omicron BA.1 and BA.2 variants [were associated] with a drop in neutralization greater in magnitude than that reported in all other variants of concern (including Beta and Delta)," and that boosting "did not completely overcome the inherent immune escape properties of Omicron."
In January 2023, the journal Cell published a study from researchers at Columbia University, which found "that [the BQ and XBB subvariants] were barely susceptible to neutralization by sera from vaccinated individuals with or without prior infection, including persons recently boosted with the new bivalent (WA1/BA.5) mRNA vaccines."
In February 2024, the journal Cell published a study by researchers from the University of Ohio, which found that "neutralizing antibodies in 3-dose-vaccinated sera [were] unable to neutralize BA.2.86 similar to XBB variants," and that "XBB.1.5-wave breakthrough infections conferred almost no [neutralizing antibodies] against BA.2.86 and FLip variants."
As of December 2024, over 4,000 SARS-CoV-2 genomes have been sampled and sequenced, and the phylogenic tree – demonstrating the exponential rate of mutation – is available on Nextstrain.org.
5. Infection impairs the CD8+ T cell response to vaccination, and breakthrough infections dysregulate T cells.
In April 2023, the journal Cell published a study by researchers at Stanford, Emory, and Harvard universities, which found "[a] decrease in the magnitude of circulating spike-specific CD8+ T cells after vaccination in recovered COVID-19 patients," which was "associated with reduced functionality, and that "this dysfunction persists for a year or more after the active phase of infection, suggesting lasting damage, despite the absence or near absence of the relevant virus." Importantly, they note that "the apparent damage of the CD8+ T cell response by viral infection is cause for concern and may leave even vaccinated individuals with a previous infection at risk for subsequent infections or other health issues."
Their results are consistent with a study by researchers at UCSF, published in Science Translational Medicine in July of the same year. According to the preprint version of the paper – quoted here because the published version is inaccessible – researchers found that "even remote, clinically mild SARS-CoV-2 infection could have long-term consequences on tissue-based immune homeostasis," and that "[long-term] T cell activation in these tissues was also observed in many individuals without Long COVID." The researchers also specified that "all but one participant had received at least one COVID-19 vaccination prior to PET imaging," and that the "median number of days from the most recent vaccine dose to tracer injection was 183 days."
In June 2021, Nature Immunology published a review article by researchers from Harvard Medical School, which describes chronic T cell stimulation and dysfunction as a common outcome in chronic infections, autoimmunity, and cancer. The article is paywalled, but accessible via Sci-Hub.
6. Breakthrough infections are not harmless.
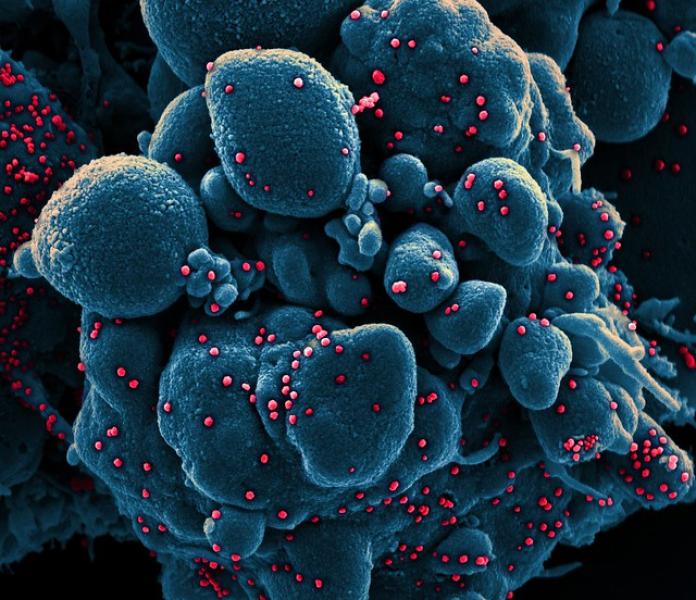
In December 2021, the journal PNAS published a study by researchers at Ohio State University, which found in vitro evidence that "the relatively robust cell-to-cell infection efficiency of SARS-CoV-2 is in part related to the higher cell–cell fusion capability of its spike protein compared with that of SARS-CoV," noting that "cell-to-cell transmission is considered to be an effective means by which viruses evade host immunity, especially antibody-mediated responses."
In July 2024, De Gruyter republished a review article in the journal Medical Review from researchers with the World Health Network. The authors note:
COVID-19 can also cause organ damage in individuals without symptoms, who would not fall under the current definition of Long COVID. This organ damage, whether symptomatic or not, can lead to various health impacts such as heart attacks and strokes. Given these observations, it is necessary to either expand the definition of Long COVID to include organ damage or recognize COVID-19-induced organ damage as a distinct condition affecting many symptomatic and asymptomatic individuals after COVID-19 infections. It is important to consider that many known adverse health outcomes, including heart conditions and cancers, can be asymptomatic until harm thresholds are reached. Many more medical conditions can be identified by testing than those that are recognized through reported symptoms. It is therefore important to similarly recognize that while Long COVID symptoms are associated with organ damage, there are many individuals that have organ damage without displaying recognized symptoms and to include this harm in the characterization of COVID-19 and in the monitoring of individuals after COVID-19 infections.
In March 2024, the journal Nature Scientific Reports published a study by researchers from multiple universities in Italy, which found that biomarkers of neuronal and glial damage remained elevated at least 10 months after both asymptomatic and clinically-mild infection in a fully vaccinated cohort. Disturbingly, as objective biomarkers of this damage decreased over the 10 month period, subjective perception of cognitive impairment increased, suggesting that the way in which the brain compensates for this damage does not improve cognitive impairment.
In August 2024, the journal ImmunoHorizons published a study by researchers at the University of Chicago, which found that "booster vaccine doses did not decrease autoantibody responses in patients with breakthrough infections, suggesting that vaccination cannot be used to combat autoimmunity resulting from exposure to SARS-CoV-2," that "autoantibody titers may not always result in immediate symptoms," and that "SARS-CoV-2 infection of any severity significantly increases the risk of developing rheumatoid arthritis, SLE, systemic sclerosis, and other rheumatic autoimmune diseases."
In December 2024, the journal Cell Host & Microbe published a study by researchers from multiple universities in Germany, which found that vaccination reduced, but did not prevent, the accumulation of SARS-CoV-2 spike protein in skull and brain tissue.
7. People who cannot access, fully benefit from, or tolerate the vaccines matter.
Immunocompromised people matter. People who are harmed by breakthrough infections, autoimmunity, and the vaccines themselves – however rare – matter.
The seemingly-immunocompetent matter. You matter. This is a virus inherently capable of evading humoral immunity, with underestimated consequences for everyone.
References:
- CDC – Effectiveness of COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Frontline Workers Before and During B.1.617.2 (Delta) Variant Predominance
- CDC – Vaccine Effectiveness Studies
- CDC – Outbreak of SARS-CoV-2 Infections, Including COVID-19 Vaccine Breakthrough Infections, Associated with Large Public Gatherings
- The Lancet Infectious Diseases – Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study
- Nature Medicine – Infectiousness of SARS-CoV-2 breakthrough infections and reinfections during the Omicron wave
- Annals of Allergy, Asthma & Immunology – Predictors of seroconversion after coronavirus disease 2019 vaccination
- Virology Journal – Seroconversion following the first, second, and third dose of SARS-CoV-2 vaccines in immunocompromised population: a systematic review and meta-analysis
- Nature Medicine – SARS-CoV-2-specific plasma cells are not durably established in the bone marrow long-lived compartment after mRNA vaccination
- Vaccine – Estimated COVID-19 vaccine effectiveness against seroconversion from SARS-CoV-2 Infection, March–October, 2021
- Nature Microbiology – SARS-CoV-2 Omicron is an immune escape variant with an altered cell entry pathway
- Cell – Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants
- Cell – Immune evasion, infectivity, and fusogenicity of SARS-CoV-2 BA.2.86 and FLip variants
- Bioinformatics/Nextstrain – Genomic epidemiology of SARS-CoV-2 with subsampling
- Cell – Spheromers reveal robust T cell responses to the Pfizer/BioNTech vaccine and attenuated peripheral CD8+ T cell responses post SARS-CoV-2 infection
-
Science Translational Medicine – Tissue-based T cell activation and viral RNA persist for up to 2 years after SARS-CoV-2 infection
- medRxiv – Multimodal Molecular Imaging Reveals Tissue-Based T Cell Activation and Viral RNA Persistence for Up to 2 Years Following COVID-19
- Nature Immunology – Not-so-opposite ends of the spectrum: CD8+ T cell dysfunction across chronic infection, cancer and autoimmunity
- PNAS – SARS-CoV-2 spreads through cell-to-cell transmission
- Medical Review – Review of organ damage from COVID and Long COVID: a disease with a spectrum of pathology
- Nature Scientific Reports – Neurofilament light chain and glial fibrillary acid protein levels are elevated in post-mild COVID-19 or asymptomatic SARS-CoV-2 cases
- ImmunoHorizons – Mild Primary or Breakthrough SARS-CoV-2 Infection Promotes Autoantibody Production in Individuals with and without Neuro-PASC
- Cell Host & Microbe – Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19
- National Academies of Sciences, Engineering, and Medicine – Evidence Review of the Adverse Effects of COVID-19 Vaccination and Intramuscular Vaccine Administration
